What is endometriosis?
Endometriosis is a condition in which the tissue that lines the uterus or womb is present on other organs. Endometriosis is usually found in the lower abdomen or pelvis, but it can appear anywhere in the body.
How do you best diagnose endometriosis?
Laparoscopy with a biopsy is the gold-standard of diagnosing endometriosis. You do need histologic confirmation by a pathologist to confirm the presence of endometrial glands and stroma on the biopsy of the specimen. The presence of an endometrioma (endometriosis filled ovarian cyst) is also diagnostic.
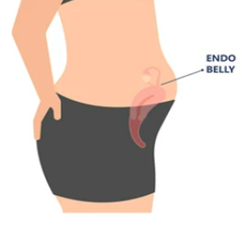
What is an "Endobelly"? This is a term for extremely painful bloating and abdominal distention that occurs in women during their period, cause
d by endometriosis. Inflammation, bowel adhesions and abnormal gut flora have all been named as culprits. Limiting inflammatory foods such as sugar, carbs, dairy, gluten, alcohol as well as breathing exercises, meditation, heat pads, warm ginger or mint tea can help.
Why is endometriosis associated with GI issues?

About 10-15% of endometriosis patients have endometriosis on their bowel which can cause painful bowel movements or even blood in the stool. Some women have bowel adhesions than can contribute to bowel symptoms. Often the bowel is stuck to other structures such as the ovaries, uterus or pelvic sidewall. This scarring can lead to pain during bowel movements or constipation or diarrhea. Other patients have SIBO or IBS, which is associated with gut dysbiosis (the imbalance of gut bacteria) and can be treated with medication and probiotics.
What is IC and why is related to endometriosis?
Interstitial cystitis and endometriosis are two separate inflammatory processes but often called the "evil twins" of pelvic pain. Up to 80% of women with endometriosis have been identified with IC. IC is when there is a defect in the bladder lining which can easily be diagnosed via a cystoscopy. It is treated with a bladder diet and medication.
What's the best treatment for endometriosis? This is different for each patient. Some patients don't want to undergo surgery and prefer medication. Some women need multiple surgeries with excision. Generally, a multimodal approach including excision surgery, hormone suppression, anti-inflammatory diet, physical therapy, and sometimes supplements, can achieve the best results.
Can you see scar tissue on imaging?
You can't directly see scar tissue, however adhesions can cause the organs in the pelvis to be less mobile, which you can assess with a "sliding test": by pushing on the uterus and ovaries, you can see if those organs move around each other (for example bladder against the uterus etc).
What is the difference between adhesions and scar tissue? Scar tissue is healed tissue. Scarring can form thicker tissue called fibrosis that can restrict movement or pull on nerves. Adhesions are scar tissue bands that form after an injury or a surgery and cause your tissues and organs to stick together. They can range from filmy to very thick. During surgery, those adhesions often need to be removed, even if not causing pain for the patient, to allow access to areas involved with endometriosis.
What is a frozen pelvis? Frozen pelvis is where all the organs are stuck together in the pelvis. Adhesions have formed from the inflammation causing ovaries, fallopian tubes, uterus, bowel, bladder all to be stuck together. Surgeries in those cases are extremely difficult and at higher risk for injury to organs or vessels. Those surgeries take a long time and should only be done by expert surgeons.
Is there anything I can do post op to prevent adhesions after surgery?
Adhesions form in the first 7 days after surgery. It can be helpful to keep tissue "mobile" after surgery. Physical therapists can do visceral manipulation and use myofascial release techniques, but immediately this can be pretty painful. Some naturopaths say that the use of Serrapeptase can prevent adhesions, but no studies have been done in endometriosis patients.

Comments